Both Testosterone and anabolic androgenic steroids (AAS) adversely influence the immune system, affecting leucocyte growth or activity, and antibody and cytokine production, particularly when used at supraphysiological doses, mimicking a condition of secondary immunodeficiency [R, R].
Secondary immunodeficiency, much more common than primary immunodeficiency (that is to say those caused by genetic defects affecting the cells of the immune system), is characterized by various factors that affect a normal immune system, including infectious, iatrogenic, metabolic and environmental factors.
These immune deficiencies are manifested clinically with an increased frequency or unusual complications of common infections and occasionally with the onset of opportunistic pathogen infections.
Nandrolone And Anadrol Effects On The Immune System
Nandrolone Decanoate and Anadrol directly induce the production of inflammatory cytokines Interleukin 1 Beta (IL-1β) and Tumor Necrosis Factor Alpha (TNF-α) in human peripheral blood leukocyte cultures [R].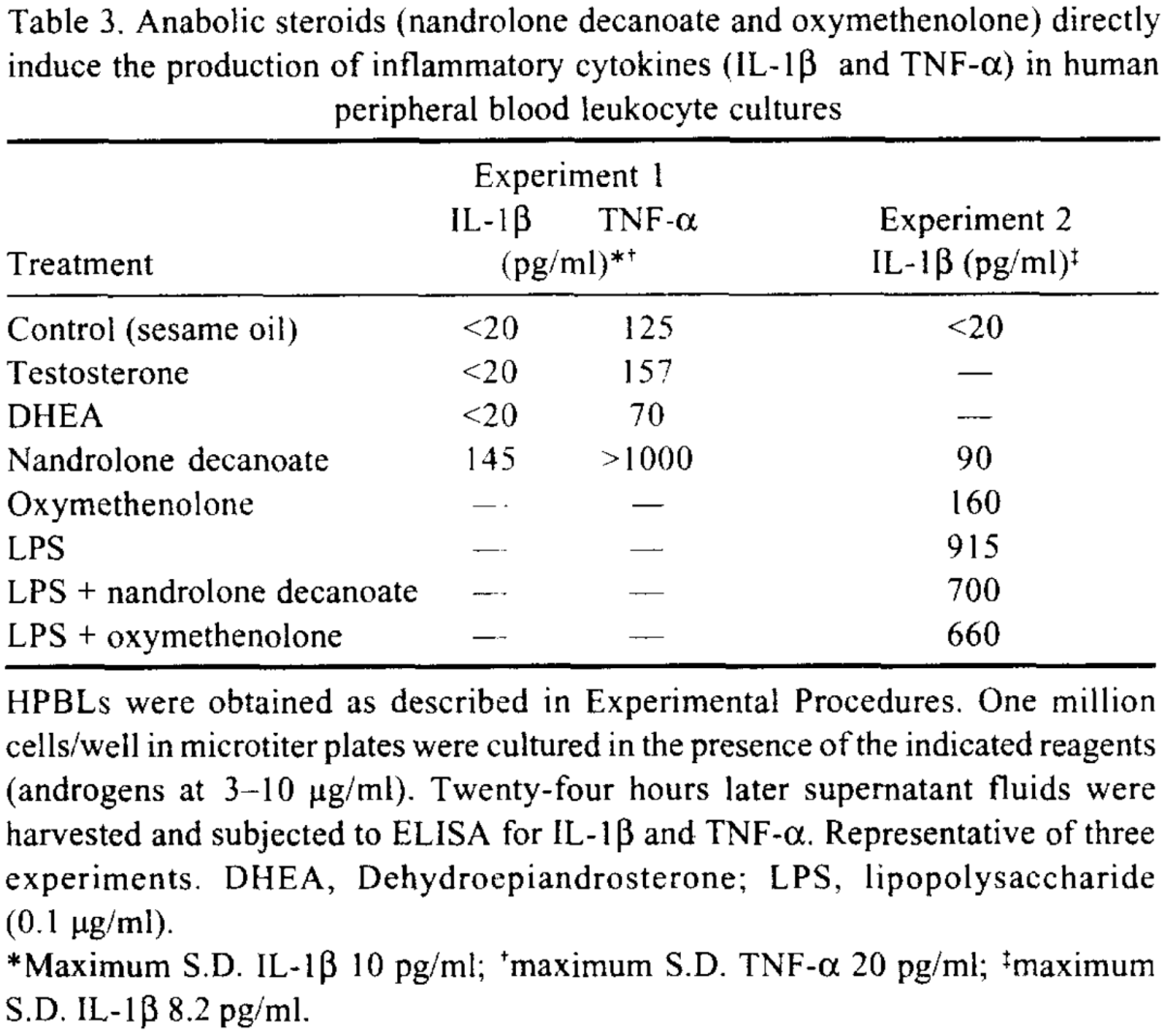
Testosterone and DHEA had no direct cytokine inducing effect in the same model.
Nandrolone Decanoate also inhibits interferon production in NDV-infected mouse L-929 and human WISH cells.
Winstrol And Trenbolone Effects On The Immune System
Winstrol and Trenbolone were found to be genotoxic and cytotoxic to human lymphocytes in a dose dependent manner [R].
Testosterone, Teslac, Anavar And Winstrol Effects On The Immune System
To evaluate how anabolic steroids affect the immune system, five commercially available steroids with various types of structural differences were studied in a rodent model [R].
Animals were divided into five groups and treated with Testosterone (group 1), Testosterone Propionate (Group 2), the steroidal aromatase inhibitor Testolactone (Teslac) (Group 3), Anavar (Group 4), and Winstrol (Group 5).
Significant immunosuppression was observed with all groups.
However, by day 10, the Teslac, Anavar and Winstrol treated group showed immunostimulation and actually exceeded baseline immunity while the Testosterone treated groups maintained immunosuppressed.
To truly test the effects of endogenous androgens on the immune system a second experiment was then performed.
Ten animals maintained in a similar manner to the initial experiment were either treated intact or were castrated and then treated for 8 days, with Anavar (1.1 mg/kg/day), Testosterone (1.1 mg/kg/day) or Anavar combined with physiologic amounts of Testosterone (15 μg/day).
Anavar was selected because it has the greatest anabolic activity of all Testosterone analogues as compared to Testosterone (androgenic/anabolic activity = 1:13).
In the intact animals after 8 days of treatment with Anavar, serum Testosterone levels were measured by radioimmunoassay on tail vein blood.
Levels were either undetectable or very low, reflecting what would be significant HPTA suppression.
Immune function (DCH responses) measured at the same time revealed a 41% increase over baseline.
The Testosterone treated group experienced a 36% suppression of immune function.
Further treatment for 8 days with Anavar combined with physiologic amounts of Testosterone eliminated the immune system enhancement provided by Anavar monotherapy and returned the DCH responses to levels that were not significantly different from baseline.
The results were different in the castrated animals.
Castration, resulted in an increase in immune (DCH) responses.
The mean observed change was 90% greater than intact (pre-castration) baseline.
That means that castrated rats had a 90% improvement above and beyond rats that weren’t castrated.
Eight day administration of Anavar to these animals had an immunodepressive effect returning the DCH response to baseline.
Eight day treatment with Anavar combined with physiologic doses of Testosterone produced an even greater suppression, 45% change from baseline.
These observations indicate that immune alterations do occur with anabolic steroids which are immunosuppressive when the steroid nucleus is intact and immunostimulatory with nuclear alterations.
How Steroids Influence Immune Function
The hypothesis to explain the immune system responses to steroids is as follows.

Exogenous androgenic anabolic steroids produce two effects on the immune system: (A) a direct early effect on immune function which is suppressive and, (B) an indirect delayed stimulatory effect mediated through the negative feedback on the pituitary.
(B) results in inhibition of gonadal Testosterone through diminished LH release.
A decrease in the synthesis of Testosterone results in low serum Testosterone level and immune stimulation.
Castration, by abolishing the modulation of Testosterone secretion eliminates the effect of (B) but leaves (A) intact.
In summation, the more suppressive a steroid is the more it can indirectly enhance immune function, simply by suppressing the endogenous production of Testosterone and its metabolites.
However, anabolic steroids will also be genotoxic and cytotoxic to human lymphocytes in a dose dependent manner.
So, the only reason anabolic steroids can enhance immunity is by being more tissue selective than Testosterone and by shutting down the HPTA, not by inherently being protective.
They too will be inherently immunosuppressive, just to a lesser degree based on their tissue selectivity and magnitude of impact on endogenous androgen production suppression.
At the end of the day, the data all suggests that the lower your levels of steroids are in the body, the higher level your immune system will function at in parallel.
Are You Increasing Your Risk Of Viral Infection When You Are On Cycle?
In summary, the vast majority of studies suggest that steroid use decreases antibody formation, Natural Killer (NK) lymphocyte activity, T and B lymphocyte maturation and stimulation resulting in immunosuppression [R].
Supraphysiological doses of common anabolic steroids have been shown to directly influence the production of certain cytokines, altering immune function.
The results from both animal and human studies suggest that supraphysiological doses of AAS can negatively impact the immune system.
The takeaway from all of this is that with an easily spread virus infecting thousands of people throughout the world right now, it would be prudent to reduce your exogenous AAS use at least down to therapeutic levels to support immune function during this time where having increased vulnerability to viral infection is the most risky.
Regardless if you are young and believe you are invincible based on the mortality rate statistics showing that the elderly are the most at risk of being symptomatic or ending up in critical condition, you may still be increasing your chances of becoming an infected carrier who then transmits the virus to the elderly (including your parents or grandparents) as a result of self-induced immunosuppression.